Understanding wisdom teeth
Wisdom tooth extraction often begins with understanding what wisdom teeth are and why they matter to your oral health. These third molars typically erupt between ages 17 and 25 in the back corners of your mouth. While some people experience no issues, others find that wisdom teeth can crowd existing teeth, lead to decay in hard-to-clean areas, or trigger painful infections [1].
Because wisdom teeth are the last to emerge, there is often limited space for proper alignment. If they grow at odd angles or only partially break through the gums, they become impacted. Impacted wisdom teeth can damage adjacent teeth, form cysts in the jaw, or create pockets where bacteria thrive, increasing your risk of infection [1].
Even if your wisdom teeth aren’t causing pain now, your dentist may recommend removal as a preventive measure. Early extraction—while roots are still small and jaw bone is less dense—tends to be safer and allows for a quicker, more comfortable recovery [1].
Determining extraction needs
Not every wisdom tooth requires removal. Your oral surgery dentist will weigh factors such as the angle of eruption, your jaw’s available space, and any signs of decay or infection. Dentists often use panoramic X-rays to assess whether wisdom teeth will cause future problems or are already impacting your oral health.
Common signs that you may need extraction include persistent pain at the back of your mouth, swelling or redness of the gums around a wisdom tooth, recurring bad breath, and difficulty opening your jaw. If you notice cysts or damage to neighboring teeth, removal becomes crucial to prevent further complications [1].
Some impacted wisdom teeth remain asymptomatic yet still pose risks. Your dentist might recommend preventive removal in your late teens or early twenties when complications are less likely and recovery is faster [1].
Preparing for extraction
Before your wisdom tooth extraction appointment, you’ll undergo a thorough evaluation with your oral surgeon. This preoperative assessment ensures that underlying conditions—such as high blood pressure or bleeding disorders—are well controlled. Your provider will review your medical history, perform imaging scans, and outline a sedation plan that suits your comfort level.
Whether you choose local anesthesia, nitrous oxide, IV sedation, or general anesthesia, it’s essential to follow these steps before surgery:
- Follow fasting instructions, typically no food or drink six to eight hours prior
- Share a list of current medications and allergies with your oral surgery dentist
- Arrange reliable transportation home, especially if you’re receiving sedation
- Wear comfortable, loose-fitting clothing and remove jewelry or contacts
- Plan time off work or school for adequate rest and recovery
By preparing carefully and choosing sedation dentistry services or consulting an implant dentist with sedation, you can reduce anxiety and make the procedure as smooth as possible.
Managing postoperative care
After extraction, your mouth needs time and specific care to heal properly. Most people experience mild bleeding, swelling, and discomfort for the first few days. Pain usually peaks around days three to four before gradually subsiding [2].
To support healing and minimize complications:
- Bite gently on gauze placed over the socket to encourage clot formation
- Apply a cold compress to your cheek intermittently for up to 48 hours
- Keep your head elevated when lying down to reduce swelling
- Avoid vigorous rinsing or spitting for 24 hours to protect the blood clot
- Stick to a soft diet—yogurt, applesauce, and mashed potatoes—avoiding hot liquids and alcohol
If you notice persistent or worsening symptoms, contact your surgeon immediately.
Common complications table
| Complication | Incidence | Warning sign | Recommended action |
|---|---|---|---|
| Dry socket | ~4% of extractions | Severe pain, exposed bone | See an OMS for a medicated dressing |
| Infection | Rare | Fever, increased swelling | Start antibiotics under professional care |
| Nerve injury | Very rare | Prolonged numbness | Follow-up with your surgeon |
| Sinus communication | Rare (upper teeth) | Sinus pain, fluid drainage | OMS evaluation and possible repair |
Evaluating oral health benefits
Removing problematic wisdom teeth does more than relieve pain—it can transform your overall oral health. By eliminating areas that trap food and bacteria, you lower your risk of gum disease and tooth decay in adjacent molars. When wisdom teeth are extracted before they cause damage, you preserve the integrity of your existing dental arch.
Extraction also simplifies daily hygiene. Flossing and brushing become easier without the back-corner crowding that often results from wisdom teeth. This streamlined care leads to fresher breath and healthier gums over time.
In cases where wisdom teeth have already harmed neighboring teeth, removal prevents further damage and may support future restorative work—such as implant-supported dentures or fixed bridges. Early intervention safeguards your smile and builds a foundation for more advanced treatments if needed.
Exploring advanced options
Some extractions present challenges—such as teeth with curved roots, limited visibility, or significant bone coverage. In these situations, you may work with an experienced oral surgery dentist who offers complex extraction & implant services.
Advanced techniques include:
- Sectioning teeth into smaller pieces for gentler removal
- Using surgical guides and magnification for precision
- Employing ultrasonic instruments to separate bone from root
These methods minimize trauma to surrounding tissues and set the stage for procedures like bone graft dental surgery when you plan future implants.
Sedation dentistry further enhances your comfort. If you’ve ever felt anxious about dental procedures, look into sedation dentistry for anxious patients or sedated tooth extraction to ensure a stress-free experience.
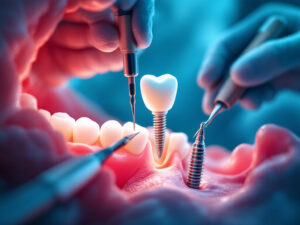
Planning implant integration
Once your extraction sites have healed, you may consider replacing missing molars with implants. Dental implants preserve bone by mimicking natural tooth roots, preventing the bone loss that often follows tooth removal.
If bone volume is insufficient, a bone graft & implant restoration procedure may be recommended. Grafting material—either from your own body or a donor source—encourages new bone growth in the jaw. Over a few months, this creates a stable platform for implant placement.
Implant placement and restoration
With bone grafts in place, an implant placement cloninger consultation will determine the ideal implant positions. Your surgeon uses 3D imaging to plan each implant’s depth and angle. This level of customization leads to better long-term success and aesthetics.
After osseointegration, where the implant fuses with bone, you’ll return for an abutment attachment and crown placement. At this stage, implant restoration services craft bespoke prosthetics that match your natural teeth. The result is a durable, life-like replacement that restores full chewing function.
For patients requiring multiple missing teeth, you might explore the all-on-4 implant procedure or a complete full mouth reconstruction. These transformative treatments combine strategic implant placement with fixed bridges or overdentures to rebuild your entire arch.
Achieving lasting oral health
Wisdom tooth extraction serves as the first step in many comprehensive dental journeys. By removing problematic third molars, you address immediate pain and infection risks while paving the way for advanced options like implants, bone grafting, and full-mouth restoration.
Whether you need a straightforward outpatient extraction or a complex surgical approach, collaborating with a skilled team—offering implant and restoration clinic services—ensures you receive state-of-the-art care. With careful planning, sedation when needed, and precise execution, your oral health can thrive for decades to come.